В настоящее время во всем мире наблюдается рост частоты проведения операций кесарева сечения. С 1960 года по настоящее время (за 5 десятилетий) отмечено 10-кратное увеличение данного вида оперативного родоразрешения [1, 2]. Подобная тенденция наблюдается и в России. По данным Федеральной службы государственной статистики частота операции кесарева сечения выросла с 17,9% в 2005 г. до 26,7% в 2014 г. В настоящее время доказано, что с увеличением числа абдоминальных родов в анамнезе женщины возрастает риск врастания плаценты [3], при этом данная патология в 75–90% сочетается с ее предлежанием [4]. Еще в 1985 году S.L. Clark и соавт. представили данные о том, что при предлежании плаценты и наличии одного рубца на матке после КС вероятность врастания плаценты составляет 24%, с увеличением числа операций в анамнезе риск возрастает и достигает 67% при наличии 4 и более рубцов [5]. Кроме того, происходящая физиологическая перестройка сосудов миометрия во время беременности, превращающаяся их в безмышечные широкие трубки, способствует кровопотере, достигающей 3000–5000 мл и более [6]. Долгое время оперирующие врачи считали необходимым отказываться от попыток отделения плаценты у пациенток с приращением во избежание массивного кровотечения, и гистерэктомия рассматривалась как обязательный атрибут при родоразрешении пациенток с истинным вращением [7–9]. В последнее десятилетие у этой категории беременных появилась надежда на сохранение матки благодаря метропластике, позволяющей избежать удаления органа. Методика заключается в реконструкции стенки матки после резекции измененного участка миометрия единым блоком с подлежащей плацентой [7, 10–12]. Для осуществления возможности проведения метропластики в первую очередь необходимо уменьшить интраоперационную кровопотерю ослабив приток артериальной крови к матке. В настоящее время существует два способа воздействия на сосудистую систему нижнего сегмента матки: экстравазально и эндоваскулярно. В первом случае производится перевязка магистральных сосудов. Однако эффективность данного воздействия едва достигает 50%, что объясняют наличием коллатерального кровоснабжения [12]. Во втором случае проводится эмболизация и/или баллонная окклюзия с эмболизацией [7, 13] магистральных сосудов. Этот метод дает возможность остановить кровотечение у 50–87% пациенток.
Наложение компрессионных швов на нижний сегмент матки доступно узкому кругу хирургов, так требует входа в подбрюшинное пространство, глубокого отделения мочевого пузыря, мочеточника, сохранения оттока из полости матки после завязывания швов и имеет высокий процент осложнений и недостаточную эффективность.
Поэтому актуальность разработки нового, простого, доступного рядовому акушеру интраоперационного метода ограничения кровопотери при кесаревом сечении по поводу предлежания плаценты очевидна.
Цель настоящего исследования – оценка эффективности комбинированной тактики с применением вагинального и маточного катетеров Жуковского при остановке послеродовых кровотечений, обусловленных врастанием предлежащей плаценты.
Материал и методы исследования
Для исследования была выделена группа из 79 беременных, у которых диагностировано предлежание плаценты с вращением. Участников исследования отбирали путем последовательной популяционной выборки.
Критерии включения: беременные с предлежанием и приращением плаценты со сроком гестации 28–42 недель.
Критерии исключения: экстрагенитальные заболевания в стадии суб- и декомпенсации, новообразования, аномалии развития половых органов, привычное невынашивание беременности, многоплодие, прерывание беременности до 28 недель, истмико-цервикальная недостаточность, инфекционные заболевания, хромосомная патология или пороки развития плода, выпадение пуповины в родах, хориоамнионит, родовая травма, прорастание приросшей плацентой параметриев, крупных сосудов.
Для оценки эффективности предлагаемого способа лечения послеродовых кровотечений при кесаревом сечении на фоне предлежания плаценты с вращением все наблюдаемые 79 пациенток были разделены на 3 группы в зависимости от лечебной тактики:
- 1-я группа контроля (n=47), в которой применялся только хирургический метод лечения – перевязка артерий, наложение гемостатического наружно-маточного сборочного шва [14, 15], иссечение вросшей дольки плаценты или резекция стенки матки (метропластика);
- 2-я группа сравнения (n=20), в которой применялся хирургический метод вместе с одним маточным баллонным катетером Жуковского;
- 3-я группа основная (n=12), в которой вместе с хирургическим методом лечения, применяли маточный и вагинальный баллонные катетеры Жуковского.
Все пациентки, включенные в исследование, были оперативно родоразрешены в плановом порядке в сроке беременности 35–36 недель.
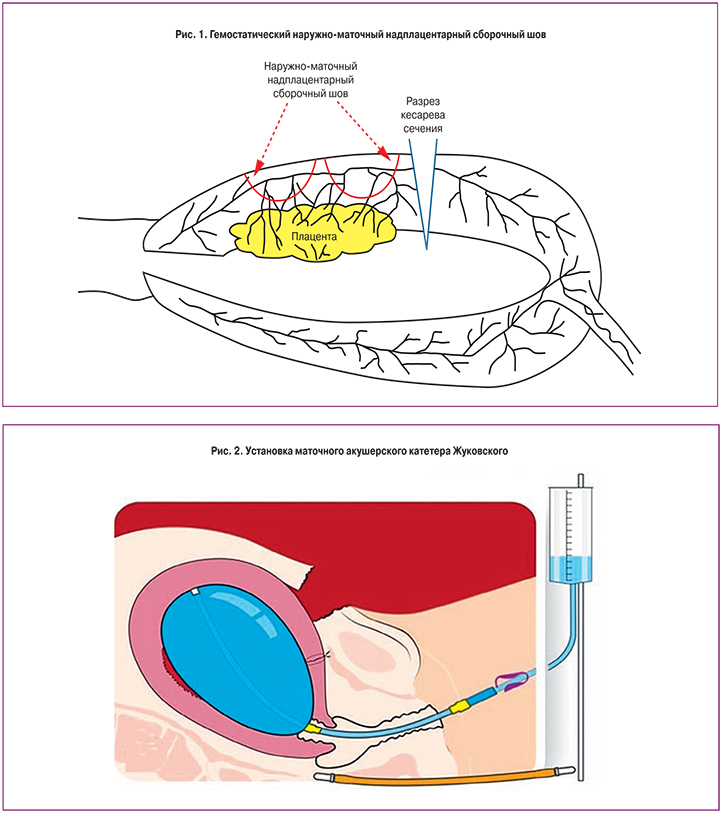
Всем пациенткам сразу после извлечения плода проводилась перевязка нисходящей ветви маточной артерии. Следующим этапом после отделения плаценты был осмотр плацентарной площадки. При обнаружении вращения плаценты на 1/3 толщины миометрия выполнялось иссечение участка вращения с одновременным лигированием кровоточащих сосудов и прошиванием плацентарного ложа ∞-образным швом. Затем выполнялась отсепаровка пузырно-маточной складки книзу и наложение гемостатического наружно-маточного сборочного шва (рис. 1) [14, 15].
При обнаружении вращения плаценты более чем на 2/3 толщины миометрия или при площади вращения более чем 5 сантиметров в диаметре выполнялось отсечение участка матки с участком вросшей плаценты, отсепаровка пузырно-маточной складки, наложение гемостатического наружно-маточного сборочного шва ниже предполагаемого отсечения стенки матки [14, 15]. В последующем проводилось восстановление стенки матки отдельными викриловыми швами.
В случае обнаружения плацентарной аневризмы проводился высокий поперечный разрез на матке для извлечения плода, затем отсечение стенки матки с вросшей плацентой и выполнение метропластики: проводилась выделение грыжевого мешка, отсепаровка пузырно-маточной складки, наложение гемостатического наружно-маточного сборочного шва ниже предполагаемого отсечения стенки матки. В последующем также проводилось восстановление стенки матки отдельными викриловыми швами.
В группе контроля после хирургического лечения дополнительные гемостатические мероприятия не проводились.
Во 2-й группе (группа сравнения) после проведения хирургического этапа интраоперационно через неушитый гистеротомический разрез, используя проводник, вводился внутриматочный катетер Жуковского (рис. 2), который наполняли физиологическим раствором после ушивания раны на матке. Продолжительность баллонной тампонады с помощью маточного катетера составляла 10–14 ч.
В основной группе (n=12) после катетеризации мочевого пузыря перед оперативным родоразрешением устанавливался вагинальный модуль (без наполнения его жидкостью), вслед за извлечением плода проводилось наполнение вагинального модуля 150 мл физиологического раствора. Дальнейшее оперативное вмешательство проводилось на фоне наполненного вагинального модуля. Следующим этапом осуществлялся хирургический гемостаз. Затем так же как и во 2-й группе устанавливали внутриматочный катетер с использованием проводника через гистеротомический разрез, проводя его через цервикальный канал. После ушивания матки маточный модуль наполняли физиологическим раствором. Продолжительность баллонной тампонады с помощью вагинального и маточного катетеров составляла 10–14 ч (рис. 3).
Для остановки кровоточивости зоны операционной раны на матке применялся местный гемостатик «Гемоблок». Методика применения: стерильные марлевые салфетки смачивали гемостатическим раствором и прикладывали к кровоточащей, предварительно осушенной поверхности раны на 3 мин.
Статистический анализ проведен при помощи Statistica 10.0.
Результаты исследования
Средний возраст женщин составил 31,6±5,5 года. Первобеременными были 19,3% женщин, в то время как первые роды предстояли 36,4% наблюдаемых. 44,3% женщин имели в анамнезе оперативное родоразрешение, 51,5% из них предстояло повторное кесарево сечение, а у 48,5% это было третье и более оперативное родоразрешение.
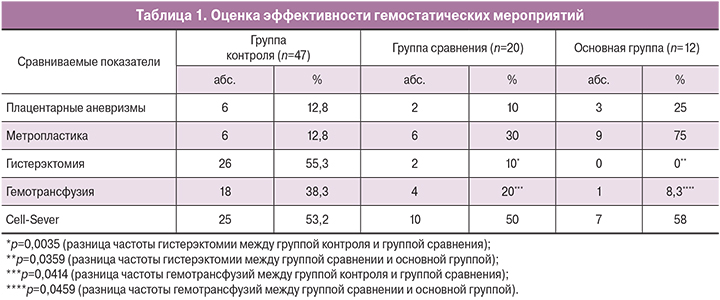
Сравниваемые группы пациенток значимо не различались по сроку беременности, акушерскому и соматическому анамнезам. Эффективность гемостатических мероприятий оценивали по объему кровопотери, частоте проведенных гемотрансфузий и количеству проведенных гистерэктомий.
В группе контроля интраоперационно в 23 случаях было выявлено врастание более на 2/3 миометрия и площадью более 5 см, у 12,8% (6/47) наблюдаемых была обнаружена плацентарная аневризма, что требовало проведения метропластики, которая была выполнена только у 6 пациенток. Несмотря на осуществленный хирургический гемостаз у 55,3% (26/47) родильниц с врастанием предлежащей плаценты имело место продолжающееся кровотечение, что потребовало для окончательной остановки кровотечения выполнения гистерэктомии.

В группе сравнения количество плацентарных аневризм составило 10% (2/20), у 6 пациенток диагностировано врастание более на 2/3 миометрия и площадью более 5 см, метропластика была выполнена в 30% случаях (6/20). При этом гистерэктомия была проведена только 10% (2/20) пациенткам. Количество органоуносящих операций в группе сравнения было в 5,5 раза ниже (р=0,0035) чем в группе контроля (табл. 1).
В основной группе у 6 наблюдаемых было обнаружено врастание более на 2/3 миометрия и площадью более 5 см, плацентарная аневризма диагностирована у 25% (3/12) женщин и после осуществления хирургического гемостаза метропластика проведена 75% пациенткам (9/12), при этом у всех родильниц кровотечение было полностью остановлено, что способствовало сохранению матки.
Проведение баллонной тампонады плацентарной площадки маточным катетером позволило сократить потребность в гемотрансфузии донорской крови в 1,9 раза (p=0,414), дополнительное введение вагинального катетера снизило необходимость в гемотрансфузии еще в 2,4 раза (p=0,0459). Достоверных различий в частоте использования аппарата Cell-Sever в исследуемых группах не было выявлено (табл. 1).
При проведении анализа кровопотери на фоне сравниваемых методов гемостаза было выявлено, что в группе сравнения где проводился только хирургический гемостаз объем кровопотери был выше (р=0,0029), чем в случае сочетания хирургического гемостаза и введения маточного катетера (рис. 4).
Та же тенденция снижения объема кровопотери была выявлена при сравнении хирургического гемостаза и его комбинации с применением двух катетеров (маточного и вагинального) (рис. 5).
При сопоставлении объема кровопотери в основной группе и группе сравнения, где использовались помимо хирургического гемостаза разные комбинации маточных катетеров, разницы объема кровопотери выявлено не было (рис. 6).
Для оценки эффективности методов интраоперационного гемостаза, была составлена таблица сопряженности (табл. 2), позволяющая установить отношение шансов потребности в проведении органоуносящих операций.
 Полученные результаты позволяют утверждать, что вероятность гистерэктомии при хирургическом гемостазе выше, чем в случаях, когда дополнительно использовался маточный катетер Жуковского. Таким образом, вероятность гистерэктомии при хирургическом гемостазе в 11 раз выше, чем при его сочетании с маточным катетером.
Полученные результаты позволяют утверждать, что вероятность гистерэктомии при хирургическом гемостазе выше, чем в случаях, когда дополнительно использовался маточный катетер Жуковского. Таким образом, вероятность гистерэктомии при хирургическом гемостазе в 11 раз выше, чем при его сочетании с маточным катетером.
Обсуждение
В соответствии с использованными в настоящей работе критериями эффективности, объем кровопотери при проведении органосохраняющих операций, осуществляемых при предлежании вросшей плаценты, был значимо ниже при сочетании хирургического гемостаза в комбинации с гемостатическими модулями Жуковского (маточный/вагинальный катетеры) в отличии то изолированно хирургического гемостаза. Разницы объема кровопотери при использовании только маточного катетера и его сочетания с вагинальным после осуществления хирургического гемостаза выявлено не было. Но, тем не менее, в основной группе, где помимо хирургического гемостаза использовалось сочетание двух гемостатических катетеров (маточного и вагинального), матку удалось сохранить у всех пациенток, в то время как в группе сравнения, где хирургический гемостаз сочетался с использованием одного маточного катетера у 10% (2/10) наблюдаемых, в связи с продолжающимся кровотечением пришлось проводить гистерэктомию.
Проведенный анализ гистологического исследования 28 удаленных маток показал, что в 25% (7/28) случаях помимо врастания ворсин хориона в миометрий были выявлены признаки гнойного эндометрита.
Использование маточного баллона в дополнение к хирургическому гемостазу позволяет снизить объем кровопотери в 1,2 раза и 11 раз уменьшить риск гистерэктомии. Однако проблема удержания баллона в пределах полости матки при осуществлении методики гемостатических мероприятий мировым сообществом акушеров оценивается как ключевое условие, определяющее ее эффективность. Вагинальный модуль способен обеспечить стабильное положение маточного баллона в полости матки за счет его прочной, максимально высокой постановки во влагалище и избежать тем самым экспульсии маточного модуля.
В отличие от зарубежных аналогов, в частности баллона Бакри, двухбаллонный катетер Жуковского обеспечивает тесное соприкосновение внутриматочного баллона и стенок матки, что препятствует накоплению крови между ними. В результате сложения разнонаправленных векторов сил, создаваемых двумя баллонами, как со стороны полости матки, так и со стороны влагалища, включаются новые механизмы остановки послеродового кровотечения. Среди этих механизмов, в первую очередь, следует отметить межбаллонную компрессию нижне-маточного сегмента.
Использование вагинального катетера Жуковского при проведении кесарева сечения на фоне предлежания вросшей плаценты позволяет остановить кровотечение из S2 сегмента за счет сдавления сети коллатералей в малом тазу, тем самым способствует выполнению органосохраняющей операции и снижает потребность в проведении гемотрансфузии. Наличие в осевой трубке вагинального модуля отверстия позволяет своевременно диагностировать продолжающиеся кровотечение и изменить лечебную тактику.
Заключение
Применение вагинального и маточного катетеров Жуковского позволяет остановить кровотечение из S2 сегмента за счет сдавления сети коллатералей в малом тазу. Данный метод позволяет выполнить органосохраняющие операции при предлежании плаценты, нижнесегметных кровотечениях, обусловленных приращением плаценты.