На современном этапе развития акушерства основными его задачами являются создание оптимальных условий для осуществления женщиной функции материнства, сохранение ее здоровья и обеспечение рождения здорового ребенка. Анализ демографической ситуации в России позволил выявить следующие особенности: крайне низкий уровень рождаемости, неудовлетворительное состояние здоровья новорожденных, высокая частота сочетания заболеваний репродуктивной сферы и экстрагенитальных заболеваний, рост осложнений беременности и родов. Вместе с тем наблюдаемая в России некоторая положительная тенденция к увеличению рождаемости привела к необходимости снижения перинатальной и детской заболеваемости и смертности, улучшению состояния здоровья будущих поколений [1].
В последние годы сфера научных интересов в перинатальной охране плода сместилась к ранним срокам беременности – к I триместру, так как именно в этот период происходит формирование фетоплацентарной системы, закладка органов и тканей плода, экстраэмбриональных структур, что в большинстве случаев определяет дальнейшее течение беременности.
Несмотря на достигнутые в последние годы успехи в профилактике и лечении, невынашивание беременности остается одной из важнейших проблем практического акушерства и наиболее частым осложнением беременности [2, 3]. В настоящее время невынашивание беременности наблюдается в 10,0–25,0% всех желанных беременностей; в I триместре оно может достигать 50,0% (по некоторым данным – до 80,0%), во II – 20,0% и в III – до 30,0% [4]. В свою очередь, по мере увеличения числа спонтанных выкидышей резко возрастает риск прерывания последующих беременностей [5].
Причины невынашивания беременности разнообразны. Хронический эндометрит сопровождает каждую четвертую даже физиологически протекающую беременность и не менее 60% – при невынашивании. Причиной возникновения хронического эндометрита могут быть инструментальные манипуляции (аборты, выскабливания полости матки и другие оперативные вмешательства), неразвивающиеся (замершие) беременности, перенесенные воспалительные заболевания органов малого таза, в том числе и сексуально-трансмиссивные заболевания [6]. В литературе обсуждается значение иммунологических причин самопроизвольного выкидыша, одной из которых является антифосфолипидный синдром [7].
В 25–57% наблюдений генез самопроизвольного выкидыша остается неустановленным [2].
 В настоящее время, несмотря на большое количество работ, доказывающих высокую эффективность прегравидарной подготовки женщин с невынашиванием беременности, в практической деятельности обследование и лечение врачу приходится осуществлять во время беременности, зачастую на поздних сроках, что не всегда позволяет устранить уже имеющиеся нарушения [8].
В настоящее время, несмотря на большое количество работ, доказывающих высокую эффективность прегравидарной подготовки женщин с невынашиванием беременности, в практической деятельности обследование и лечение врачу приходится осуществлять во время беременности, зачастую на поздних сроках, что не всегда позволяет устранить уже имеющиеся нарушения [8].
Таким образом, одним из аспектов повышения рождаемости является анализ невынашивания беременности на ранних сроках, а перспективным направлением для научного поиска является разработка эффективных, обоснованных и безопасных схем комплексного лечения и профилактики невынашивания беременности.
Прогестерон − один из основных гормонов в организме женщины, который обеспечивает регулярный менструальный цикл, играет важную роль в процессах наступления и сохранения беременности. В названии − «progestatio» («для беременности») отражена основная точка приложения действия этого гормона: децидуальные превращения эндометрия и подготовка его к имплантации, усиление васкуляризации миометрия, стимуляция роста и развития молочных желез.
Первые работы о возможности сохраняющей терапии с помощью прогестинов появились в 1953 г. По данным современных авторов, в 64–89% случаев основным патогенетическим механизмом невынашивания становится недостаточность прогестерона или снижение рецептивности эндометрия к действию этого гормона [9].
Дефицит прогестерона сказывается соответственно на децидуализации эндометрия и повышает сократимость матки. Из клинического опыта Ж.К. Ди Ренцо (2015) большинство выкидышей (75%) связано именно с нарушением имплантации. В I триместре 23–60% спонтанных выкидышей происходит из-за недостаточности лютеиновой фазы. Другим важным фактором является иммунный ответ организма матери, который играет ключевую роль во время имплантации. При невынашивании нарушения иммунной толерантности организма матери по отношению к плоду ответственны за 15–20% выкидышей [5].
Значение прогестерона для сохранения и развития беременности определило его место в профилактике и лечении угрозы аборта. Прямым показанием для лечения прогестероном является недостаточность желтого тела, то есть состояние, сопровождающее значительное число как спонтанных, так и индуцированных беременностей или беременностей, получаемых с помощью вспомогательных репродуктивных технологий [10, 11].
Уже накоплен огромный пласт данных, доказывающих эффективность производных прогестерона в лечении различных форм невынашивания беременности. Однако и сегодня продолжается поиск оптимальных препаратов на основе прогестерона, которые могли бы применяться в акушерстве с ранних сроков беременности и отвечать высоким требованиям безопасности.
Цель исследования: оценить эффективность включения микронизированного прогестерона праджисан в комплекс мероприятий по профилактике и лечению невынашивания в ранние сроки гестации.
Материал и методы исследования
В исследование включены 30 женщин, получавших лечение угрозы прерывания беременности с I триместра (I группа), и 32 женщины с клиникой угрозы прерывания беременности, отказавшиеся от лечения по различным причинам (II группа). Диагноз «угроза прерывания беременности» ставился на основании жалоб и ультразвуковой диагностики (укорочения шейки матки и расширения внутреннего зева). Исследование выполнено в соответствии с международными нормативами и правилами GCP.
Критерии включения в исследование: репродуктивный возраст (18–45 лет); одноплодная беременность; кровянистые выделения из половых путей; ретрохориальная гематома по данным ультразвукового исследования; срок гестации до 12 недель. Критерии исключения: возраст младше 18 лет и старше 45 лет; многоплодная беременность; сахарный диабет и эндокринные заболевания в стадии декомпенсации; миома матки больших размеров; аномалии развития половых органов; беременность в результате ЭКО; мужской фактор бесплодия.
Наблюдение за течением беременности осуществлялось в соответствии с требованиями приказов Министерства здравоохранения и социального развития Российской Федерации № 572н от 2012 г. и включало общеклиническое и лабораторно-инструментальное обследование, которые проводились в необходимом количестве в установленные сроки. При наличии показаний со стороны матери или плода, проводились дополнительные исследования.
 Всем беременным проводилось ультразвуковое исследование (УЗИ). Ультразвуковыми показателями угрозы прерывания беременности были укорочение шейки матки до 25 мм и расширение внутреннего зева.
Всем беременным проводилось ультразвуковое исследование (УЗИ). Ультразвуковыми показателями угрозы прерывания беременности были укорочение шейки матки до 25 мм и расширение внутреннего зева.
Для коррекции возникших осложнений гестации женщины с угрозой прерывания беременности получали терапию, включающую: санацию влагалища с коррекцией микробиоценоза, токоферолы и фолаты, препараты для нормализации стула. Для лечения угрозы прерывания беременности с ранних сроков был назначен микронизированный прогестерон (праджисан) – 200 мг интравагинально, ежедневно, в два приема (утром и вечером) до 20-й недели гестации. В качестве критериев эффективности лечения анализировали переносимость, безопасность (нежелательные явления, их связь с использованием препарата), оценку самой женщиной, особенности течения беременности. Отказавшиеся от лечения сами или по совету врача получали альтернативную терапию.
Статистический анализ полученных данных проводился на персональном компьютере, в качестве программного обеспечения использовался пакет модулей для статистической обработки данных Statistica for Windows 8.0 (StatSoft Inc., США, 2010).
Результаты исследования
Возраст обследованных женщин колебался от 18 до 30 лет, что соответствует оптимальному возрасту реализации репродуктивной функции женщин. Результативность терапии оказалась высокой: сократилось число пациенток с мажущими выделениями с 33 (53,2%) до 3 (10%) в I группе и до 18 (56,3%) – во II группе. Если до лечения на боль внизу живота и в области поясницы жаловались 53 (85,5%) женщин с угрозой прерывания, то в I группе по окончании курса терапии – только у 5 (16,7%), а во II – 25 (78,1%).
Отдельное внимание было обращено на ультразвуковые параметры (рис. 1), указывающие на диагностику угрозы невынашивания, а именно: длину шейки матки, область внутреннего зева, наличие ретрохориальных гематом, преимущественную локализацию плаценты, расстояние от нижнего края плаценты до внутреннего зева. Расширение внутреннего зева более 10 мм зарегистрировано у 2 (6,7%) женщин с угрозой прерывания беременности из группы получавших терапию осложнений гестации и у 9 (28,1%) отказавшихся от госпитализации.
Длина шейки матки менее 25 мм зафиксирована у 12 беременных: 2 (6,7%) из I и 10 (31,3%) из II группы. Краевое прикрепление плаценты выявлено у 4 (13,3%) и 9 (28,1%) соответственно, а ультразвуковые признаки ретрохориальной гематомы – у 2 (6,7%) и 4 (12,5%) беременных соответственно.
В результате микроскопического исследования содержимого влагалища 62 женщин в ранние сроки беременности у 23 диагностирован бактериальный вагиноз, у 19 – кандидозный вульвовагинит и у 20 – неспецифический вульвовагинит. Результаты восстановления микроэкологии гениталий оценивались по основным показателям бактериологического и бактериоскопического исследования.
При микроскопическом исследовании содержимого урогенитального тракта у пролеченных женщин наблюдалась нормализация флоры: в умеренном количестве определялись лактобациллы, исчезала грамотрицательная микрофлора, отсутствовали споры и мицелий дрожжевых грибов рода Candida. Слизь в отделяемом из половых путей обследованных женщин после терапии не определялась или присутствовала в небольшом количестве без патологических включений. По данным контрольного микроскопического исследования у 18 (60,0%) пролеченных пациенток количество лейкоцитов не превышало 5 в поле зрения и более 20 лейкоцитов в поле зрения обнаружено лишь у 3 (10%). При микроскопическом исследовании после лечения «ключевые клетки» обнаружены у 2 (6,7%) пациенток, ни в одном случае не выявлены споры и мицелии грибов.
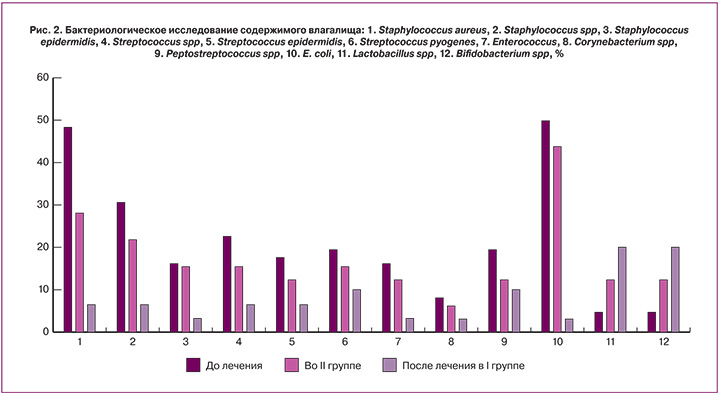
По данным бактериологического исследования после лечения отмечалось качественное и количественное улучшение микрофлоры влагалища в группе получавшей лечение в сравнении с той, которые отказались от него (рис. 2).
Выявлено снижение общей обсемененности половых путей, что отражало нормализацию микробиоценоза. Это же обстоятельство подтверждалось при детализации данных по изучению микрофлоры гениталий обследованных пациенток. Частота высевания E. Coli до лечения была высокой, но после терапии значительно уменьшалась, наблюдалось снижение величины обсемененности урогенитального тракта Prot. vulg., Prot. mirab. Частота высева Staph. Aureus, Str. pyog. до лечения превышала аналогичные показатели после лечения.
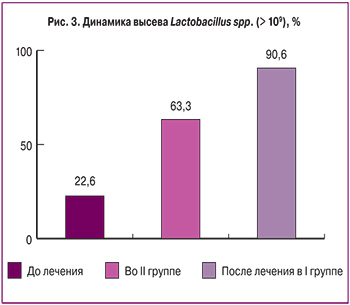
Примечательно, что только у 14 (22,6%) женщин до начала терапии в содержимом вагины определялись лактобациллы. Существенным признаком восстановления биоценоза у женщин с дисбиозом гениталий в ранние сроки гестации является увеличение частоты высева лактобактерий. В группе пролеченных женщин отмечено их значительное увеличение – до 90% (рис. 3).
Отсутствие лечения возникших осложнений у женщин во II группе явилось следствием осложненного дальнейшего течения беременности, по сравнению с пациентками I группы, которым лечение было начато еще в I триместре. У двух женщин (6,3%) из II группы, не получавших своевременную и адекватную терапию возникших осложнений, беременность завершилась поздним самопроизвольным абортом на 16–18-й неделе, дальнейшее наблюдение за ними прекратилось.
Закономерным итогом данного сценария явилось более частое развитие угрозы преждевременных родов во II группе по сравнению с I группой (р<0,05). Угроза преждевременных родов в I группе была выявлена у 3 (10%) женщин из группы получавших терапию осложнений беременности, что было в 2,6 раза реже по сравнению с II группой 10 (31,3%). У трех женщин из II группы произошли преждевременные оперативные роды на 31–33-й неделе гестации (9,4%), один новорожденный умер в первые сутки жизни.
Обсуждение
Включение микронизированного прогестерона праджисан в в комплекс мероприятий, направленных на сохранение и пролонгирование беременности, показало высокую эффективность у пациенток с угрозой невынашивания беременности. 29 из 30 женщин с угрожающим выкидышем (96,7%) в I группе (группе праджисана) беременность удалось сохранить и пролонгировать до срока доношенной беременности, в то время как во II группе (отказавшихся от лечения) – только у 19 (59,4%). Также было показано, что своевременное восстановление влагалищного биоценоза способствует нормализации течения беременности.
Данные УЗИ также подтверждали наши выводы о том, что течение беременности усугубляется в отсутствие своевременной коррекции возникших осложнений. По данным УЗИ у женщин, отказавшихся от терапии, достоверно чаще диагностировалось укорочение шейки матки менее 25 мм и расширение внутреннего зева более 10 мм, в два раза чаще обнаруживались нарушение расположения хориона (низкое) и визуализировалась ретрохориальная гематома по сравнению с группой пациенток, получавших терапию.
Заключение
Таким образом, лечение с объективно доказанной угрозой прерывания беременности препаратом микронизированного прогестерона праджисан можно оценить как высокоэффективное – беременность сохранилась и прогрессировала у 96,7% женщин. Микронизированный прогестерон праджисан является эффективным, безопасным и патогенетически обоснованным средством лечения женщин, имеющих риск прерывания беременности с ранних сроков.