В настоящее время имеются убедительные данные, доказывающие, что генитальная инфекция выступает триггером многих осложнений гестации и причиной неблагоприятных перинатальных исходов [1–5]. Вызывая локальный и системный воспалительный ответы, инфекционные агенты могут стать причиной прерывания беременности на любом сроке, формирования плацентарной недостаточности, восходящего инфицирования и перинатальной патологии [6–13]. Особенно актуальными остаются вопросы, касающиеся патогенеза и своевременной диагностики внутриматочной инфекции (ВМИ) или внутриматочного воспаления во время беременности, которым сегодня отводится ведущая роль в генезе преждевременных родов [14–20]. Учитывая, что объективным критерием ВМИ может служить только гистологическое исследование тканей последа, продолжается поиск неинвазивных критериев диагностики ВМИ во время беременности с целью своевременного назначения лечебно-профилактических мероприятий.
 Цель исследования: выявить клинико-иммунологические критерии ВМИ.
Цель исследования: выявить клинико-иммунологические критерии ВМИ.
Материал и методы исследования
Проведено проспективное обследование 327 беременных женщин на сроке 12–16 недель. Набор пациенток велся методом сплошной выборки, из обследуемой когорты были исключены беременные, имеющие следующие состояния: 1) инфекционные гепатиты, сифилис, ВИЧ-инфекция; 2) аутоиммунные заболевания; 3) экстрагенитальная патология в стадии декомпенсации; 4) индуцированная и многоплодная беременность. Комплексное обследование включало клинико-лабораторные, микробиологические и иммунологические методы исследования (показатели клеточного и гуморального иммунитета, уровень интерлейкинов и сигнальных молекул в периферической крови и цервикальной слизи). После родов у обследованных женщин проводилось морфологическое исследование последов с выявлением признаков ВМИ (воспалительно-клеточная инфильтрация в различных структурах плаценты).
Статистическая обработка полученных данных осуществлялась с помощью статистического пакета Statistica 8.0 (StatSoft, USA). Для создания прогностической модели был использован Roc-анализ и регрессионный анализ с построением модели логистической регрессии, метод построения – пошаговый с включением переменных в модель, рассчитывались коэффициенты уравнения регрессии В и exp(В), показатели чувствительности и специфичности [21, 22].
 Результаты исследования
Результаты исследования
По результатам морфологического исследования последов признаки ВМИ были зарегистрированы в 39,7% случаев (130 женщин). Для каждого клинического показателя, ассоциированного с наличием ВМИ, был рассчитан относительный риск (OR) (рис. 1). Самым значимым фактором риска ВМИ является наличие цервицита (OR=8,33). Анализируя анамнестические факторы риска, мы выявили, что выкидыши, два аборта и более, неразвивающаяся беременность, преждевременные роды увеличивают риск ВМИ в 1,38–2,3 раза, воспалительные заболевания органов малого таза (ВЗОМТ) в анамнезе – в 2,44 раза, использование внутриматочной контрацепции (ВМК) – в 2,12 раза. Наличие хронических очагов инфекции (заболевания ЛОР органов и мочевыделительной системы), острые инфекционные заболевания во время настоящей беременности увеличивают риск ВМИ в 1,58–2,23 раза. Стойкая угроза прерывания беременности, по-видимому, является одним из самых частых проявлений ВМИ, повышая ее риск в 2,14 раза. Отклонения от нормы в структуре плаценты и количестве околоплодных вод по данным ультразвукового исследования (УЗИ) увеличивают тот же риск в 1,9 раза, а нарушение маточно-плацентарного кровотока (НМПК) – в 1,78 раза. Для выбора наиболее значимых независимых предикторов наличия ВМИ мы провели регрессионный анализ. Перед включением в модель переменные «выкидыши в анамнезе», «неразвивающаяся беременность в анамнезе», «2 аборта и более в анамнезе», «преждевременные роды в анамнезе» были объединены в одну переменную «отягощенный акушерско-гинекологический анамнез» (ОАГА).
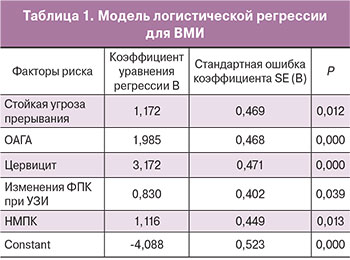
Построение модели было остановлено на пятом шаге. R2 модели составил 0,447, р<0,00001. Коэффициенты уравнения логистической регрессии приведены в табл. 1. В модель вошли пять переменных: ОАГА, наличие цервицита, изменения в фетоплацентарном кровотоке (ФПК) по данным УЗИ, НМПК, стойкая угроза прерывания беременности.
Значимость каждого критерия в данной модели сопоставима друг с другом. Для упрощения использования данных показателей в клинической практике на основе построенной регрессионной модели мы создали шкалу, в которой каждому критерию был присвоен 1 балл.
Шкала диагностики ВМИ у беременных женщин:
- ОАГА – 1 балл;
- Цервицит – 1 балл;
- Изменения ФПК при УЗИ – 1 балл;
- Стойкая угроза прерывания беременности – 1 балл;
- НМПК – 1 балл.
Для изучения диагностической ценности предложенной нами шкалы мы исследовали риск ВМИ у 327 женщин обучающей выборки, а также у 60 женщин контрольной выборки (табл. 2). Как следует из данных таблицы, риск ВМИ при отсутствии всех предикторов (0 баллов) составляет 8,3%, а при наличии 4–5 баллов морфологические признаки ВМИ обнаруживаются у 88,9–100% беременных. При наличии 1–3 баллов риск ВМИ составляет от 23,4 до 75,9% и требует дальнейшего обследования беременной.
Наряду с клиническими показателями мы изучили диагностическую ценность отдельных иммунологических показателей в качестве критериев прогноза ВМИ. При сравнении результатов иммунологического обследования у женщин с наличием и отсутствием ВМИ статистически значимые различия были получены по следующим показателям периферической крови: общему количеству лейкоцитов и моноцитов, лизосомальной активности нейтрофилов и моноцитов, активности и интенсивности фагоцитоза моноцитов, уровню интерлейкинов (IL)-1β, IL-8, IL-17, IL-10, sVE-кадгерина и α-дефензинов. При изучении показателей цервикальной слизи статистически значимые различия обнаружены в общем количестве лейкоцитов, функциональной активности нейтрофилов, уровне IL-10, IL-4, интерферона (IFN)-γ, sVE-кадгерина и α-дефензинов. Повышение количества лейкоцитов в периферической крови более 12×109/л, не связанное с инфекционными процессами экстрагенитальной локализации, было обнаружено у половины пациенток с ВМИ, специфичность данного показателя составила 98,2%, чувствительность – 54,2%.
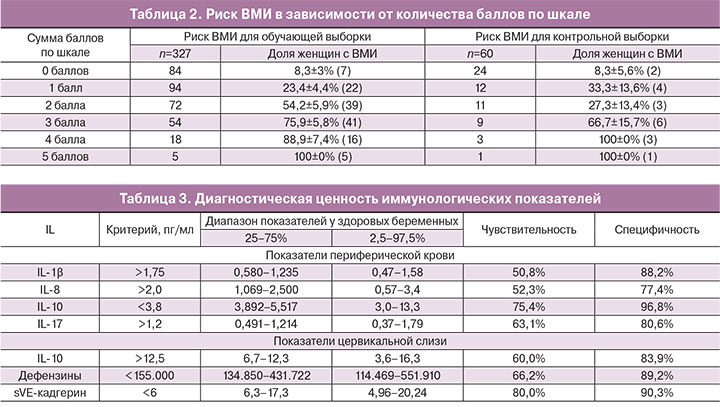
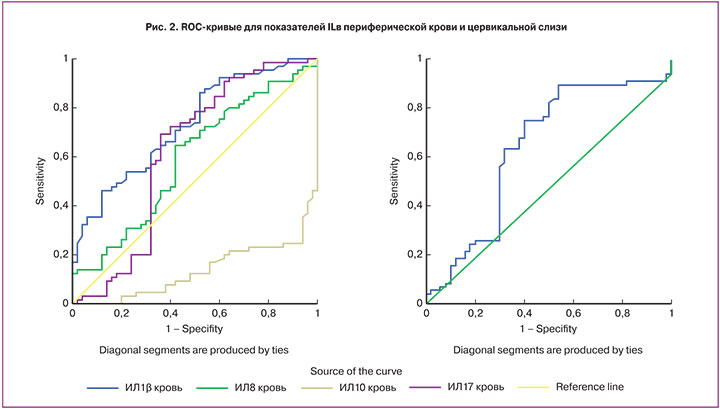
На основании анализа ROC-кривых мы отобрали семь иммунологических показателей с максимальной AUC, выбрали точки разделения для каждого показателя, оценили диагностическую ценность данных тестов, а также сопоставили выбранные нами значения с диапазоном значений аналогичных показателей, полученных у 30 здоровых беременных женщин (физиологическое течение беременности, отсутствие генитальной инфекции и морфологических признаков ВМИ) (табл. 3, рис. 2).
Наилучшими признаками чувствительности и специфичности обладали показатели IL-1β, IL-10, IL-17. Критический уровень IL-1β для диагностики ВМИ находится за пределами как интерквартильного диапазона, так и 95% диапазона соответствующего показателя у здоровых беременных. Критические уровни IL-8, IL-10, IL-17 выходят за пределы интерквартильного диапазона, но остаются в пределах 95% диапазона для здоровых лиц. Учитывая, что понятие «нормы» в медицине является сложной и дискуссионной проблемой, мы рекомендуем использовать найденные нами показатели в качестве ориентиров при диагностике ВМИ, принимая во внимание, что данные уровни цитокинов в небольшом проценте случаев могут встречаться и у здоровых беременных.
Из показателей цервикальной слизи наибольшей диагностической ценностью обладают уровни IL-10, sVE-кадгерина и α-дефензинов. Значение диагностического критерия для IL-10 (>12,5 пг/мл) выходит за пределы интерквартильного интервала, но остается в пределах 95% диапазона для здоровых беременных, что несколько снижает его диагностическую ценность. Чувствительность и специфичность для уровня sVE-кадгерина <6 61="" 81="" 2="" -="" 155="" 000="" 66="" 2="" 89="" 2="" p="">
Обсуждение
Разработанная нами 5-балльная шкала критериев ВМИ позволяет с большой долей вероятности поставить данный диагноз во время беременности с целью проведения своевременных лечебно-профилактических мероприятий. Клиническими критериями, входящими в шкалу, являются: наличие цервицита у беременных с ОАГА (2 и более искусственных аборта, досрочное прерывание предыдущих беременностей), стойкая угроза прерывания, ряд эхографических признаков (изменение структуры плаценты, аномальное количество околоплодных вод), НМПК. Воспалительный процесс шейки матки, выступивший как один из значимых критериев ВМИ, может, с одной стороны, являться маркером наличия хронического эндометрита у женщин с ОАГА, с другой стороны, стать причиной несостоятельности факторов антимикробной защиты на уровне шейки матки, способствуя тем самым восходящему инфицированию. Изменения в состоянии ФПК, НМПК свидетельствуют о формировании хронической плацентарной недостаточности инфекционного генеза. При наличии 4–5 баллов морфологическое подтверждение ВМИ имеет место у 88,9–100% беременных. При сумме 1–3 балла риск ВМИ составляет 23,4–75,9%, требуя дальнейшего обследования беременной. В качестве дополнительного обследования могут выступать иммунологические показатели периферической крови и цервикальной слизи, самыми значимыми из которых являются: в периферической крови – IL-1β>1,75 пг/мл; IL-10<3,8 пг/мл; IL-17>1,2 пг/мл; в цервикальной слизи – sVE-кадгерин <6 -="" 155="" 000="" p="">
Таким образом, состояние системного и локального иммунитета у беременных женщин с ВМИ, с одной стороны, характеризуется некоторым повышением их провоспалительного потенциала, с другой, отражает снижение функциональной активности отдельных звеньев системы врожденного иммунитета. В периферической крови у пациенток с ВМИ имеет место доминирование провоспалительного потенциала над иммуносупрессорным, дополнительным доказательством которого является снижение уровня IL-10. Наши данные совпадают с результатами исследований других авторов [11]. Учитывая имеющиеся знания о механизмах, ответственных за активацию сокращения гладкомышечных клеток матки, выявленный дисбаланс таких цитокинов, как IL-1β и IL-10, может стать одной из причин преждевременного прерывания беременности на фоне ВМИ. Уменьшение уровня sVE-кадгерина (адгезивных молекул, экспрессируемых в эндотелиальных клетках) в цервикальной слизи у женщин с ВМИ, возможно, свидетельствует о его усиленной интернализации с поверхности эндотелия, следствием чего является повышение проницаемости эндотелия для нейтрофилов. Известно, что нейтрофилам цервикального секрета принадлежит ведущая роль в антимикробной устойчивости гениталий [3]. Снижение активности антимикробных пептидов (α-дефензинов) в цервикальной слизи, главными продуцентами которых являются нейтрофилы, может быть следствием их «функционального истощения» и отражать неполноценность противоинфекционной защиты на уровне шейки матки. Такая неполноценность локального иммунного ответа повышает потенциальную возможность «прорыва» шеечного барьера и восхождения инфекции в верхние отделы генитального тракта.
Заключение
Использование данных клинико-анамнестических и иммунологических критериев ВМИ во время беременности может служить основанием для прогнозирования акушерских и перинатальных осложнений и проведения этиопатогенетических лечебных мероприятий.