В связи со сложившейся в настоящее время тенденцией изменения структуры инфекционных болезней урогенитальной сферы все большее значение приобретают микроорганизмы, патогенные потенции которых слабо учитывались здравоохранением [1–3]. К таким заболеваниям относится Candida-инфекция урогенитального тракта (вульвовагинальный кандидоз), удельный вес которой среди урогенитальных инфекций у женщин составляет 20–70% [4, 5] и продолжает расти [6].
С учетом наблюдаемой тенденции к росту заболеваемости грибковыми инфекциями, их социальной значимости, а также росту резистентности возбудителей к антимикотикам вопрос выбора средств противогрибковой терапии приобретает особую актуальность [1, 7].
Несмотря на появление в последнее время значительного количества антимикотиков различных групп, эффективное лечение кандидозов из-за быстрого развития резистентности и возможности повторного инфицирования остается проблематичным. Еще одной проблемой, играющей немаловажную роль в поддержании инфицирования влагалища, является точка зрения, согласно которой роль в рецидивировании вульвовагинального кандидоза может играть очаг дрожжевых грибов Candida, локализующийся в толстом кишечнике человека [2, 5]. При этом использование триазоловых соединений, с целью санации кишечника от грибов не вполне оправданно – около 80% активных их метаболитов выводятся с мочой, а в кишечной биопленке они не концентрируются; при этом при использовании данного соединения у 2/3 пациентов полной санации кишечника достичь не удается [1, 8]. В то же время не имеющий системной абсорбции натамицин, который действует только в просвете толстого кишечника, представляется в данной ситуации оптимальным выбором.
Одним из наиболее известных и распространенных классов антимикотиков являются полиеновые макролиды, продуцируемые микроорганизмами рода Streptomyces соединения [5]. К преимуществам полиеновых макролидов можно отнести крайне редко встречающуюся резистентность грибов [1, 5, 9], а также высокий профиль безопасности при их местном применении [5, 9, 10]. Наиболее часто применяемым полиеновым макролидом с антимикотическим действием является натамицин [5, 8, 11]. Натамицин является единственным представителем класса полиеновых макролидов, механизм действия которого связан не с образованием пор в мембране гриба, а с ингибированием экзо- и эндоцитоза, слияния вакуолей и функционирования белков-переносчиков, что лишает гриб энергетических субстратов и способности к размножению, при этом наряду с метаболическими нарушениями взаимодействие натамицина с эргостерином приводит и к отчетливым морфологическим изменениям грибковой клетки [5, 9, 12]. Еще одно важное свойство натамицина – отсутствие влияния на репродуктивную функцию и внутриутробное развитие, что дает возможность применять его препараты в период беременности и лактации [10].
Цель исследования: оценка метода терапии беременных женщин, больных вульвовагинальным кандидозом, с сочетанием перорального и интравагинального введения полиенового макролида – натамицина (кишечнорастворимые таблетки и вагинальные суппозитории пимафуцин, ЛЕО Фарма, Дания).
Материал и методы исследования
В период нашей работы наблюдалось 110 беременных женщин в сроке гестации 10–12 недель больных вульвовагинальным кандидозом (ВВК). Исследования проводились на кафедре акушерства, гинекологии и перинатологии ФГБОУ ВО Кубанский государственный медицинский университет Минздрава России, в женских консультациях г. Краснодара. Всем женщинам проведено обследование согласно приказу № 572н от 12.11.2012 г. Министерства здравоохранения Российской Федерации.

Диагностику инфицированности различными видами Candida spp. проводили несколькими методами: прямая микроскопия (соскобы со слизистой влагалища, вульвы и цервикального канала (использовались неокрашенные и окрашенные по Граму препараты), также определялся pH среды влагалища; посев с выделением чистой культуры и окончательная идентификация возбудителя (автоматизированная система «API 20 C Aux», BioMerieux, Франция). Для оценки эффективности терапии методом случайной выборки все пациентки были разделены на две репрезентативные группы: I группа (55 пациенток), получавших терапию полиеновым макролидом (натамицин) вагинальные суппозитории в дозе 100 мг 1 раз в сутки в течение 6 дней; II группа (55 пациенток), получавших терапию полиеновым макролидом (натамицин) интравагинально в дозе 100 мг 1 раз в сутки в течение 6 дней + пероральное введение натамицина (таблетки, покрытые кишечнорастворимой оболочкой) в дозе 100 мг 4 раза в сутки в течение 10 дней.
Ввиду того, что группы по всем исследованным параметрам были однородными, нами без определения достоверной массовой доли каждого исследуемого признака, для суждения о клиническом состоянии больной была предложена интегральная субъективно-объективная балльная оценка (0 баллов – отсутствие симптома, 1 балл – средняя степень выраженности симптома, 2 балла – выраженная симптоматика). Это позволяет в динамике оценивать, как интенсивность каждого симптома, так и суммарную интегральную балльную оценку клинической картины. Результаты исследований были обработаны методом вариационной статистики с определением критерия Фишера (F) для оценки непараметрических показателей групп малых выборок и критерием Стьюдента (t) для независимых групп. Анализ проводился с использованием программы Statistica 6.0.
Результаты исследования
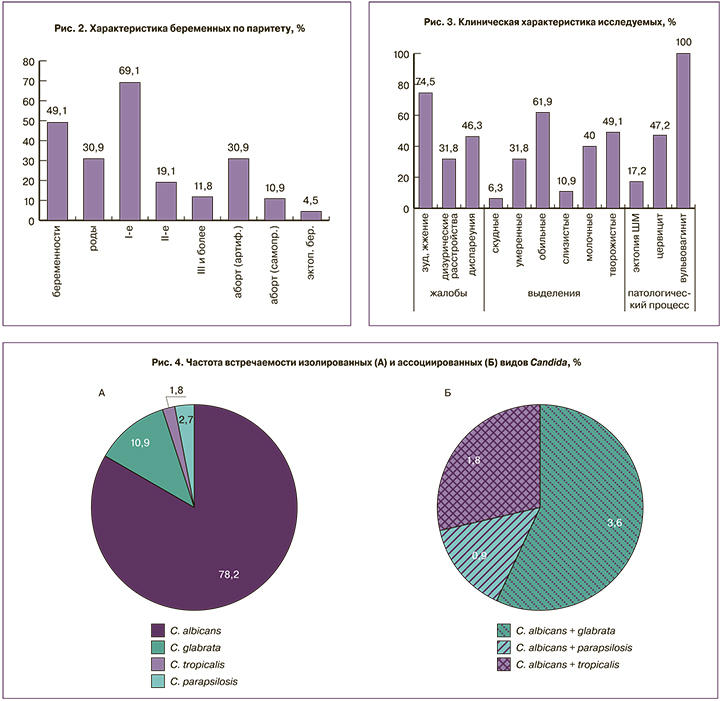
Анализ полученных данных показывает, что прямой зависимости заболеваемости вульвовагинальным кандидозом от возраста, семейного положения, места работы и других социальных причин выявлено не было (рис. 1). Средний возраст менархе составил 13,2±0,2 года. Средний возраст полового дебюта – 18,1±0,3 года. Беременности в анамнезе имели 49,1% пациенток, из них рожавшие – 30,9%, имели артифициальные аборты также – 30,9% беременных (рис. 2).
У беременных с признаками вульвовагинального кандидоза был проведен анализ ранее перенесенных и ныне сопутствующих хронических соматических и гинекологических заболеваний как факторов, влияющих не только на состояние влагалища, иммунный статус, но и на различные звенья репродуктивной системы женского организма. По анамнезу количество перенесенных инфекционных заболеваний в детском и пубертатном периодах у них было выше, чем в популяции (инфекционный индекс 1,5). Из соматической патологии было выявлено достаточное количество хронических заболеваний желудочно-кишечного тракта (колит – 10,9%, гастрит – 19,1%, холецистит – 7,3%, дисбактериоз кишечника – 34,5%). Гинекологическая заболеваемость анамнестически составила 49,1%.
Все больные женщины, включенные в выборку, в той или иной степени имели определенные клинические проявления (рис. 3). Превалировали жалобы на выделения из половых путей в повышенном количестве «слизисто-молочного» и «творожистого» характера, субъективные ощущения в виде зуда, жжения, болей при мочеиспускании, болезненности полового акта. При объективном исследовании отмечались изменения слизистых, характерные для вульвовагинального кандидоза (отечность, гиперемия слизистой оболочки влагалища и вульвы, иногда изъязвления и трещины в области наружных половых органов), мацерация половых губ и аногенитальной зоны, лейкоцитоз в мазках из влагалища и цервикального канала, а также обнаружение мицелия или собственно клеток дрожжевых грибов рода Candida.
Показатели pH-метрии вагинального отделяемого отмечались в пределах 3,5–6,0 (в среднем 4,7±0,01).
 Таким образом, можно констатировать, что вульвовагинальный кандидоз у значительного количества беременных протекает с выраженной симптоматикой, что согласуется с данными отечественных и зарубежных исследований [13, 14].
Таким образом, можно констатировать, что вульвовагинальный кандидоз у значительного количества беременных протекает с выраженной симптоматикой, что согласуется с данными отечественных и зарубежных исследований [13, 14].
Основным возбудителем вульвовагинального кандидоза у обследованных беременных (110 пациенток) была Candida albicans (рис. 4А-Б), она обнаружена (самостоятельно и в ассоциациях) у 84,5% пациенток, на втором месте по распространенности оказалась Candida glabrata, которая самостоятельно и в ассоциациях с C. albicans выявлена у 14,5%) больных ВВК, Candida tropicalis и Candida parapsilosis (самостоятельно и в ассоциациях с C. albicans) определялись соответственно в 3,6% для каждого из видов.
Таким образом, наше исследование подтвердило ведущую роль в этиологии вульвовагинального кандидоза Candida albicans. При этом необходимо учитывать значение Candida glabrata, которая еще 5 лет назад обнаруживалась лишь в единичных случаях, в настоящее время также должна учитываться в клиническом и терапевтическом плане. Если по нашим исследованиям количество non-albicans штаммов грибов рода Candida составляет порядка 15%, по данным зарубежных авторов оно доходит до 35% [6, 8]. При этом препараты азолового ряда не действуют на значимую часть non-albicans [12, 14]. Устойчивостью или сниженной чувствительностью к азоловым антимикотикам обладают, в частности, C. krusei, C. glabrata, C. tropicalis и ряд других.
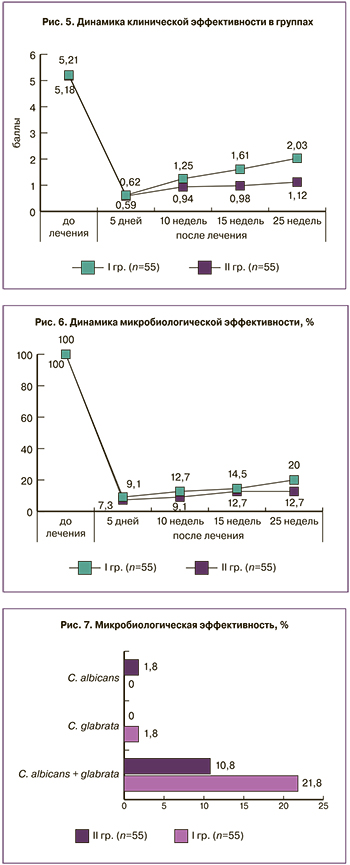
Через 5 дней после окончания терапии натамицином в обеих группах отмечено достоверное (P<0,005) и практически одинаковое снижение суммы баллов клинической оценки как в I группе, в которой беременные получали только местную антимикотическую терапию (в 8,4 раза), так и во II группе, где к интравагинальному введению натамицина был добавлен его пероральный прием (в 8,6 раза) (рис. 5). Данный факт доказывает высокую клиническую эффективность натамицина при лечении вульвовагинального кандидоза во время беременности. Учитывая, что одной из особенностей течения вульвовагинального кандидоза во время беременности является его частое рецидивирование, мы провели оценку клинической и микробиологической эффективности через 10, 15 и 25 недель от момента окончания терапии. Выявлено, что возвращение клинической картины вульвовагинального кандидоза через 10 недель после окончания терапии по сумме баллов в 1,7 раза чаще (1,65±0,13 против 0,94±0,11 балла соответственно; P<0,001) происходило в группе, в которой не проводилась пероральная терапия натамицином. Через 15 и 25 недель, несмотря на то что в обеих группах увеличилось количество беременных с симптоматикой вульвовагинального кандидоза, в I группе балльная оценка клинических признаков в данный период составила соответственно 1,61±0,12 и 2,03±0,14, во второй группе данный показатель был 0,98±0,11 и 1,12±0,13.
Таким образом, в клиническом аспекте отмечали достоверно (P<0,05) более высокую эффективность комплексного лечения натамицином (пероральный прием в сочетании с вагинальными суппозиториями) по сравнению с только локальной терапией натамицином.
Микробиологическое исследование в обеих группах проводили через 5 дней, 10, 15 (микроскопия) и 25 недель (микроскопия и культуральный метод) после окончания терапии (рис. 6). В результате исследования выявили, что через 5 дней после проведенной терапии в I группе микробиологическая санация (клинически значимое отсутствие в мазках мицелия и клеток грибов рода Candida) обнаружена у 90,9% беременных, во второй группе результат был аналогичным (92,7%).
Через 10 недель после окончания лечения грибы рода Candida выявлены у 12,7% пациенток I и 9,1% II группы. В дальнейшем разница в количестве пациенток с выявленным грибом рода Candida возросла в I группе до 20,0%, а во второй до 12,7% (медиана в I группе составила 14,1±1,6, во II – 10,4±1,3).
Культуральный метод с идентификацией возбудителя, проведенный через 25 недель после окончания лечения, выявил, что в I группе Candida albicans идентифицирована у 21,8% пациенток, у 1 (1,8%) женщины обнаружена Candida glabrata. Во II группе Candida albicans выявили у 10,9% пациенток, у 1 (1,8%) пациентки присутствовала ассоциация Candida albicans и Candida glabrata (рис. 7).
Обсуждение
Терапия вульвовагинального кандидоза, сопровождающаяся одновременной санацией толстого кишечника может расцениваться как патогенетически обоснованная, поскольку биоценоз влагалищной микробиоты тесно взаимосвязан с биоценозом кишечника. Ранее различными авторами была многократно показана статистическая корреляция избыточного интестинального роста Candida spp. и вульвовагинального кандидоза [15, 16]. Дополнительное назначение таблеток натамицина для применения внутрь с целью санации кишечника позволяет снизить рецидивирование вульвовагинального кандидоза и добиться более стойкого эффекта. Натамицин обладает высоким профилем безопасности в виду его низкой абсорбции, что было отмечено в различных исследованиях за более чем 50-летний опыт применения препарата [17, 18]. Минимальная системная абсорбция натамицина имеет немаловажное значение при подборе терапии для беременных женщин, поскольку, в сравнении с другими противогрибковыми средствами, обладающими более высокой системной абсорбцией, позволяет минимизировать риск для плода.
В России натамицин в лекарственной форме «суппозитории вагинальные» и «кишечнорастворимые таблетки» разрешен к применению с I триместра беременности, что позволяет рекомендовать его женщинам с вульвовагинальным кандидозом, находящимся на ранних сроках беременности.
Заключение
Полученные данные подтверждают клиническую и микробиологическую эффективность сочетания интравагинального и перорального применения натамицина у беременных с вульвовагинальным кандидозом в I триместре. Зарубежный и отечественный опыт сочетанного перорального и интравагинального применения натамицина у беременных позволяет рекомендовать такую схему с целью минимизации рецидивирования.